Salter-Harris Fractures
Dr. Elizabeth Lehto
Case
An 8-year-old male presents with pain in his distal right arm after falling from a hoverboard onto an outstretched arm. He has no swelling or obvious deformity to arm but is very tender with palpation over the distal radius. There are no abrasions or lacerations, and patient is neurovascularly intact. Imaging shows no evidence of fracture. Despite negative imaging, you are still concerned that patient has a fracture. You wonder what to do next.
Introduction
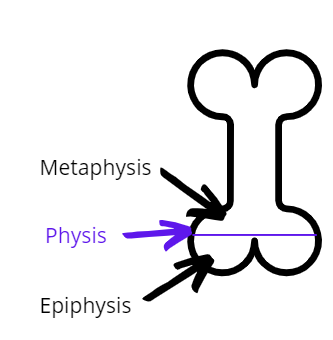
Salter-Harris fractures are fractures that involve the physis (growth plate) of long bones. The physis is an area of cartilage that actively develops into new bone, increasing the bones length. Because the area is actively growing, it is prone to fracture. Thus, Salter-Harris fractures are the most common type of pediatric fracture. These fractures are important to recognize because they can lead to growth arrest if they are not diagnosed and treated promptly.
The Salter-Harris classification was proposed by Salter and Harris in 1963 and is the most widely used system for describing physeal fractures. Conveniently, Salter-Harris type fractures can be remembered by the mnemonic SALTER.
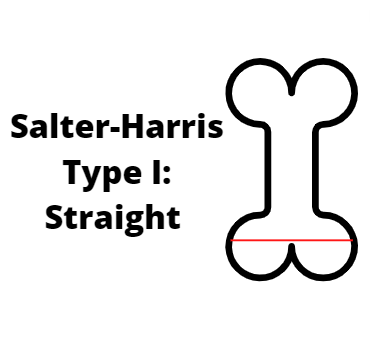
Salter-Harris Type I: Straight
Fracture is straight through the growth plate and doesn’t involve the bone.
Accounts for 5-7% of physeal fractures. The x-ray may be normal, and diagnosis is often clinical with tenderness to palpation over the growth plate. This fracture type has good prognosis.
The affected area should be splinted. Plain radiographs obtained at least seven days after injury will show healing bone. This also proves a definitive diagnosis.
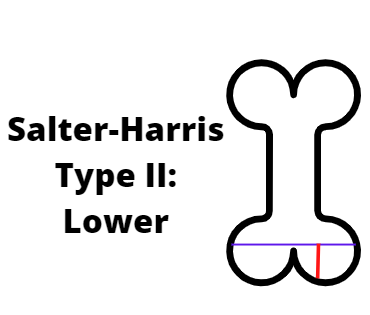
Salter-Harris Type II: Above
Fracture involves the physis and the metaphysis.
This is the most common type of physeal fracture, accounting for about 75% of physeal fractures. This fracture type has good prognosis.
Treat by cast or splinting the involved area. Displaced fractures should undergo closed reduction. Image should be repeated in 7-10 days to assess healing.
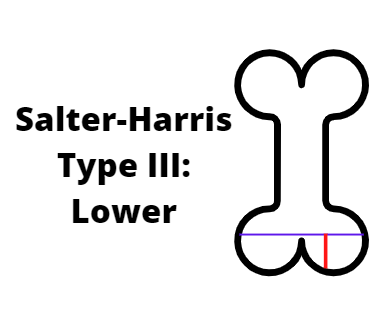
Salter-Harris Type III: Lower
Fracture involves the physis and epiphysis.
This fracture type accounts for 7-10% of physeal fractures. This fracture type has poor prognosis as the proliferative and reserve zones are interrupted.
Typically requires open reduction and internal fixation. Image should be repeated in 7-10 days to assess healing.
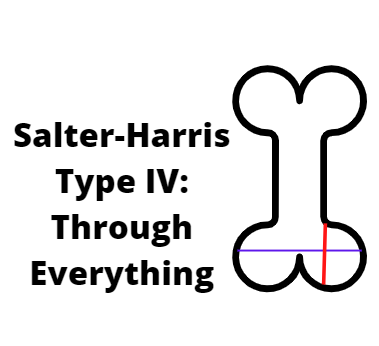
Salter-Harris Type IV: Through Everything
Fracture through the metaphysis, physis, and epiphysis.
Accounts for 10% of physeal fractures. This fracture type has poor prognosis as the proliferative and reserve zones are interrupted.
Typically requires open reduction and internal fixation. Image should be repeated in 7-10 days to assess healing.
Salter-Harris Type V: Rammed
Crush injury of the growth plate.
Accounts for less than 1% of physeal fractures. This fracture type has the worst prognosis. Growth arrest and partial physeal closure are common.
Emergent orthopedic consultation should be obtained as soon as this fracture type is recognized.
One More Mnemonic:
The SALTER mnemonic is a helpful way to remember the different types of fractures. However, can sometimes be confusing, especially given there is a physis on each end of the bone.
Another helpful mnemonic for Salter-Harris type II-IV is MEME.
Salter-Harris Type II: Metaphysis
Salter-Harris Type III: Epiphysis
Salter-Harris Type IV: Metaphysis and Epiphysis
Back to the Case:
Given patient has tenderness to palpation over the distal radius and no apparent fracture on imaging, you are concerned about a Salter-Harris type I fracture. You place the patient in a splint and discharge home. On repeat imaging one week later there is evidence of remodeling across the physis, confirming the diagnosis.
Elizabeth Lehto, D.O.
University of Louisville | UL · Department of Pediatrics | Doctor of Pediatric Emergency Medicine
Dr. Elizabeth Lehto is a Pediatric Emergency Medicine Attending at Norton Womens and Children’s Hospital. Dr. Lehto attended Midwestern University Arizona College of Osteopathic Medicine and completed her residency and fellowship at the University of Louisville.
References:
Brown, J. H., & DeLuca, S. A. (1992). Growth plate injuries: Salter-Harris classification. American family physician, 46(4), 1180–1184.
Cepela, D. J., Tartaglione, J. P., Dooley, T. P., & Patel, P. N. (2016). Classifications In Brief: Salter-Harris Classification of Pediatric Physeal Fractures. Clinical orthopaedics and related research, 474(11), 2531–2537. https://doi.org/10.1007/s11999-016-4891-3
Larsen, M. C., Bohm, K. C., Rizkala, A. R., & Ward, C. M. (2016). Outcomes of Nonoperative Treatment of Salter-Harris II Distal Radius Fractures: A Systematic Review. Hand (New York, N.Y.), 11(1), 29–35. https://doi.org/10.1177/1558944715614861
Levine RH, Foris LA, Nezwek TA, et al. Salter Harris Fractures. [Updated 2022 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430688/
Su, A. W., & Larson, A. N. (2015). Pediatric Ankle Fractures: Concepts and Treatment Principles. Foot and ankle clinics, 20(4), 705–719. https://doi.org/10.1016/j.fcl.2015.07.004
Yao, J., Bai, R., Zhao, A., & Wang, S. (2021). The "Hand as Foot model" in Salter-Harris classification of epiphyseal injury in children. Asian journal of surgery, 44(11), 1432–1433. https://doi.org/10.1016/j.asjsur.2021.07.034