Health Equity
Dr. Elizabeth Lehto
In your medical practice, be it in the clinic, hospital, or emergency department, you may have noticed that some patients seem to be hospitalized more often or have a harder time managing their health. For example, some patients with diabetes have a harder time keeping their blood glucose under control than others, or some patients are more likely to have a heart attack than others.
You may have even noticed some patterns among these patients, such as patients from certain neighborhoods tend to be hospitalized more frequently for asthma.
When treating patients, you may wonder what can be done to better help these patients. While individual cases may vary, the answer often lies in working towards systemic changes to ensure health equity.
What is Health Equity?
Health equity means that everyone has a fair and just opportunity to be healthy. This requires removing obstacles to health, such as poverty and discrimination, and their consequences, including powerless and lack of access to good jobs, quality education and housing, safe environments, and health care.1
Overcoming these obstacles is rarely something a person can do on their own. Instead, it requires adaptive change from the government, health care organizations, and communities to reduce (and ultimately eliminate) health care disparities.1
Health care disparities do not have a single cause, instead they are created and maintained through multiple interconnected and complex pathways, including:2
Social determinants of health
Poverty
Access to education
Racism
Discrimination
Environmental and community conditions
Advertising
Violence
Air quality
Transportation
Grocery stores
Parks
Behavioral factors
Diet
Tobacco use
Physical activity
Availability and quality of medical services
Equity vs Equality
When designing programs, there may be debate about focusing on achieving equality or equity.
Equality provides the same resources to everyone. For example, a primary care office that wants to empower patients to monitor their blood pressure at home may provide everyone with a free blood pressure cuff and instructions on how to use it.
Equity means that people have opportunities based on their needs, which allows everyone to have access to the same level of health. For example, a clinic that charges for visits on a sliding scale based on income so that patients have access to care regardless of their ability to pay.
While it may seem that projects should be designed around equality, it is not always preferable as it pays little attention to the desired outcomes.
For instance, a clinic may want to decrease the rate of foot infections in their patients with diabetes. They feel that if their patients are better able to control their blood glucose, they will develop fewer infections. Therefore, they implement a program that provides provide free glucose monitors and testing strips to all their patients diagnosed with diabetes.
While this program treats everyone equally, it may not have the desired outcome. Patients who hadn’t been checking their glucose previously may be more likely to monitor their glucose levels, especially those who previously had difficulty obtaining these supplies through monetary or transportation concerns. However, patients who are unable to afford their medications or who live in an area with limited access to healthy nutritious foods are unlikely to see the same benefit.
Promoting Health Equity
While health disparities can be addressed at multiple levels, the greatest achievements have relied on the use of laws, regulations, and environmental improvement strategies.2 Physicians play an important role in these improvements though community engagement, needs identification, and implementation/evaluation of evidence-based interventions including:2
Policy improvements: laws, regulations, and administrative action. For example, regulations regarding the nutrition content of school lunches.
System improvements: Changes that impact social norms of an organization or institution. For example, integration of tobacco screening and referral process into the electronic medical record.
Environmental improvement: changes to the physical, social, or economic environment. For example, adding sidewalks to enhance connectivity and promote physical activity.
These interventions have the potential to affect a large portion of the population. However, without careful design and implementation, interventions may inadvertently widen health inequities.2 Therefore, it is important to keep in mind that: 2
Different strategies require varying levels of individual or community effort and resources, which may affect who benefits and what rate they benefit
Certain populations may face barriers or negative unintended consequences which can limit the strategy’s effect and worsen the disparity
Groups experiencing health disparities have further to go to attain their full health potential than those who are not experiencing disparities, so even with equitable implementation health effects may vary
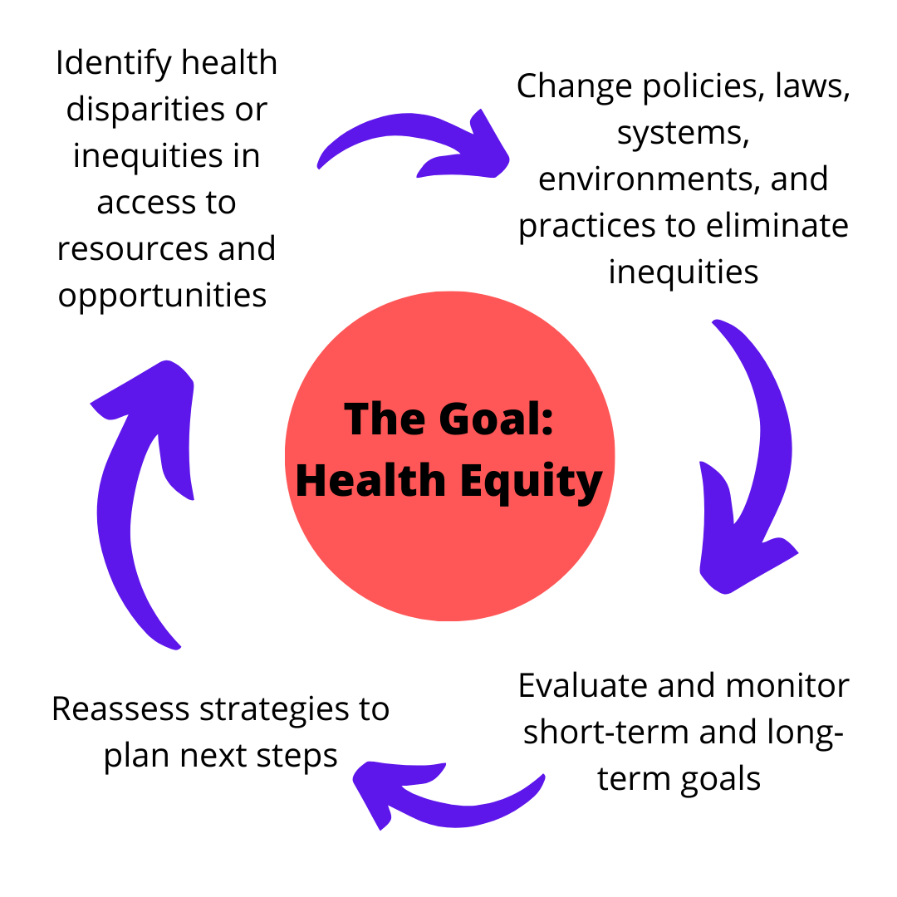
Key Steps to Promoting Health Equity
Adapted from: Braveman P, Arkin E, Orleans T, Proctor D, and Plough A. What Is Health Equity? And What Difference Does a Definition Make? Princeton, NJ: Robert Wood Johnson Foundation, 2017.
Projects designed to promote health equity often begin by identification of health disparities. While at times the cause of a disparity may be known, such as the association between poverty and obesity, at other times the cause is not yet known. Work can still be done to address these disparities for which the cause isn’t known.
When designing programs to address healthcare disparities it is important to engage the target group to identify and address their health equity goals. Successful approaches address multiple factors at a time, including improving socioeconomic resources and building community capacity to address obstacles to health equity.1
While the ultimate goal is to eliminate disparities while improving health outcomes, it is important to identify short and intermediate term goals to show an initiative is working. Gaps should be assessed using both absolute measures (such as percentage of adults in each group that develop type 2 diabetes in a 5-year span) and relative measures (such as adults in one group are X times as likely to develop type 2 diabetes than adults in another group).1 Disadvantaged groups should be compared to more advantaged groups rather than the population as a whole. This is because when the disadvantaged group represents a sizable portion of the population, comparing the disadvantaged group to the whole population compares the group largely with itself and underestimates the size of the gap between the disadvantaged and advantaged.1
Programs should be reassessed periodically, and changes made as needed. This is an important step to ensure that the program is working and does not inadvertently widen health inequities. For example, anti-smoking campaigns inadvertently led to widened socioeconomic disparities in smoking because the untargeted messages were picked up and applied more readily by those who were more affluent and had more education.1 Engaging the target community is one way to help increase the likelihood that the project helps the community in the way it is intended.
Community Engagement
Involving community members in health initiatives can foster connectedness and trust, enhance the effectiveness of programs, and increase sustainability of programs. Some things to consider to enhance community engagement: 2
Understand Historical Context: Examining the history of the community as well as past engagement efforts can be helpful to understand issues and to learn what has worked or has been less successful in the past.
Build Community Relationships Early On: Authentic community engagement takes time and requires an ongoing commitment from all involved. It is often helpful to establish and maintain strong relationships with communities before searching for funding opportunities to help with project sustainability.
Engagement Techniques: Different community engagement techniques may be used based on the purpose of the engagement as well as the resources available. Examples of engagement activities include interviews with community members, focus groups, forums, assessment mapping, and community member participation on boards or councils.
Understand and Address Barriers to Community Participation: Community members often have many demands and may be unclear about the value of their involvement to the project. Having a clear and agreed upon purpose for engagement may be helpful and shows that community members time and efforts are being respected. Efforts should be made to conduct meetings in community members native languages or to provide interpretation or other services to address language and cultural barriers to participation. Engagement activities should take place at times and places that are convenient to the community. It can be helpful to provide transportation or childcare services.
Support and Build the Community’s Capacity to Act: Activities should be chosen that increase the community’s awareness of health inequities and proved sills on how to intervene as well as cultivate members of the community as leaders and support local coalitions. These efforts can serve a community beyond one project and can also position community members and organizations to apply for additional funding to help sustain efforts.
Summary
Health equity is something that takes time and effort to address. By modeling and promoting health equity, individuals and organizations can improve healthcare for those living with health disparities. While health disparities can be addressed at multiple levels, the greatest achievements have relied on the use of laws, regulations, and environmental improvement strategies. When designing projects, it is essential to engage the target community in every stage of the project to ensure that their needs and goals are being met and to ensure longevity of the project. Programs should be reassessed periodically and adapted if goals are not being met.
Additional Resource
American Public Health Association: https://www.apha.org/topics-and-issues/health-equity
Centers for Disease Control and Prevention: https://www.cdc.gov/chronicdisease/healthequity/index.htm
Elizabeth Lehto, D.O.
University of Louisville | UL · Department of Pediatrics | Doctor of Pediatric Emergency Medicine
Dr. Elizabeth Lehto is a Pediatric Emergency Medicine Attending at Norton Womens and Children’s Hospital. Dr. Lehto attended Midwestern University Arizona College of Osteopathic Medicine and completed her residency and fellowship at the University of Louisville.