Trouble Breathing and Vomiting. Is it a Panic Attack, or is it…Anaphylaxis?
Dr. Elizabeth Lehto
Case
18-year-old female presents to the emergency department (ED) with concern for facial flushing, difficulty breathing, and vomiting. She was at a party with some of her friends when she developed flushing and difficulty breathing after eating a cookie. Friends thought she may be having a panic attack, so took her outside where she had several episodes of emesis. Symptoms did not improve, so she was brought to the ED for evaluation.
On arrival, patient has facial flushing and diffuse wheezing. She is complaining of abdominal cramping. She is unsure of the contents of the cookie she ate when symptoms began. She admits she gets anxious at times but has never had a panic attack before. Patient asks if she is having a panic attack, but you tell her you suspect something else is going on.
What is Anaphylaxis?
Anaphylaxis is a life-threatening systemic reaction caused by the sudden release of mediators from mast cells and basophils. Symptoms typically occur within minutes of exposure, however, delayed reactions have been reported. Anaphylaxis is often underrecognized and undertreated. The goal is early recognition and treatment to prevent progression to airway compromise or circulatory collapse.¹
Diagnosis:
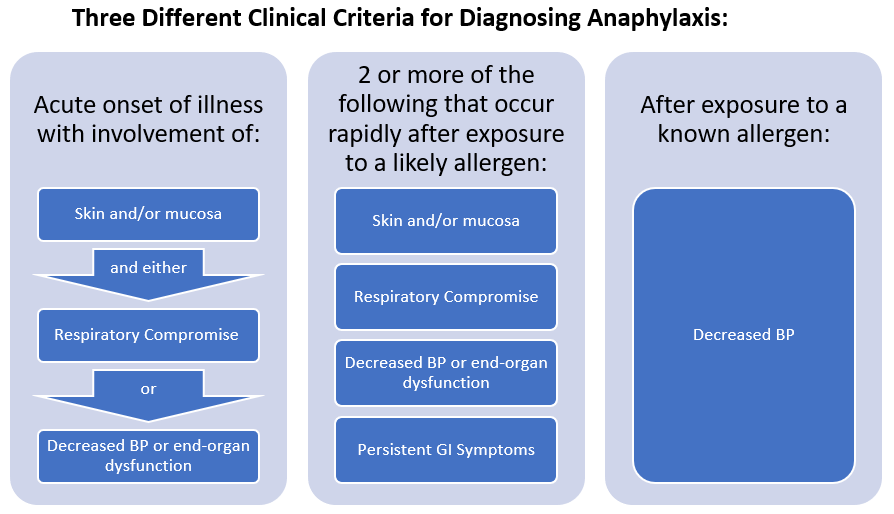
Anaphylaxis is a clinical diagnosis, and is likely when any of the three criteria are met:²
1. Acute onset of an illness (minutes to several hours) with involvement of:
Skin and/or mucosa: pruritus, flushing, hives, angioedema
AND EITHER
Respiratory compromise: dyspnea, wheeze/bronchospasm, decreased peak expiratory flow, stridor, hypoxemia
OR
Decreased blood pressure (BP) or end-organ dysfunction: collapse, syncope, incontinence
2. Two ore more of the following that occur rapidly after exposure to a likely allergen:
Skin and/or mucosa: pruritus, flushing, hives, angioedema
Respiratory compromise: dyspnea, wheeze/bronchospasm, decreased peak expiratory flow, stridor, hypoxemia
Decreased BP or end-organ dysfunction: collapse, syncope, incontinence
Persistent gastrointestinal intestinal (GI) symptoms: vomiting, cramping abdominal pain, diarrhea
3. Decreased Blood pressure after exposure to a known allergen to the patient
What Are Some Common Causes of Anaphylaxis? ¹,³
Food: 90% of reactions are caused by eight common allergens, with peanuts and tree nuts causing most fatalities in the United States
Milk
Egg
Soy
Wheat
Peanut
Tree nut
Fish
Shellfish
Medications:
Penicillin (most common cause)
Cephalosporins
Aspirin
Non-steroidal anti-inflammatory drugs (NSAIDs)
Chemotherapy
Insect bites or stings
Yellow jackets
Wasps
Hornets
Bees
Black ants
Fire ants
Latex
Vaccine components
Latex
Egg
Gelatin
Neomycin
Exercise
Idiopathic: Up to 20% of reactions
Okay, My Patient Definitely Has Anaphylaxis, Now What?
Epinephrine is the first line of treatment for anaphylaxis. The recommended dose is 0.01 mg/kg of the 1 mg/mL solution (1:1,000 solution), maximum of 0.3 mg in children and 0.5 mg in adults.¹,³
An intramuscular (IM) injection into the mid-anterolateral thigh is preferred regardless of age. This has been shown to have more rapid and higher rise in plasma concentration compared to the subcutaneous route.¹ IM epinephrine can be repeated every 5-15 minutes.
Remember, there is no contraindication to IM epinephrine in anaphylaxis. If you suspect anaphylaxis give epinephrine!
Patients who remain hypotensive or continue to have poor perfusion following IM epinephrine or who need multiple doses of IM epinephrine may need intravenous (IV) epinephrine.
Bolus doses of IV epinephrine can be used in adults but must be used with caution. In general, this should only be used in patients who are suffering cardiovascular collapse that is refractory to IM epinephrine and volume resuscitation and an epinephrine infusion is not available. This is done by giving a slow infusion of 0.05 mg to 0.1 mg of the 0.1 mg/mL solution (1:10,000 solution) over 5-10 minutes. Note, this dose is significantly less than used in cardiac arrest.⁴
A continuous IV epinephrine infusion may be needed. A 1 mcg/mL solution is used for IV infusions. Starting dose is 0.1 mcg/kg/minute and increased by 0.05 mcg/kg/minute until BP and perfusion improve. The maximum dose in children is 1 mcg/kg/minute.⁴
My Patient is in Distress, What Can be Done While Epinephrine is Being Drawn Up?
Don’t forget to monitor the patient’s airway, breathing, and circulation. Administer oxygen as needed. Patients who have marked stridor or respiratory arrest should be intubated immediately. Be prepared for early intubation in patients who have voice changes or swelling of their lips, tongue, or uvula. Anticipate a difficult airway due to swelling. Patients who are hypotensive should be given a bolus of normal saline (20 mL/kg in children, max 1,000 mL). This can be repeated, however if there is persistent hypotension an epinephrine infusion may be needed.
What about Second Line Therapies?
There isn’t much literature on adjunctive therapies for anaphylaxis, and most of the data is extrapolated from other conditions. However, when a patient presents in anaphylaxis one can consider giving albuterol, antihistamines, and/or steroids.²,⁴,⁵
Albuterol: Consider in patients with wheezing that does not respond to epinephrine
Antihistamines: Typically used to alleviate itching and mucocutaneous symptoms. Combining H1 and H2 blockers may be more effective than using H1 blockers alone. Typically, diphenhydramine and famotidine are used.
Steroids: Thought to prevent the biphasic rection, however no clear evidence. Steroids are frequently given because of known efficacy for other allergic diseases.
What is the Biphasic Reaction?
The biphasic reaction is return of symptoms after a patient is asymptomatic for more than one hour without being re-exposed to the antigen. This generally occurs in the first 4-6 hours, however, can occur up to 72 hours later. 20% of patients have a biphasic reaction. It is typically less severe than the initial reaction.⁴
I’ve Given Epinephrine and My Patient is Stable, How do I Decide Disposition?
Patients with mild to moderate episodes that respond promptly to epinephrine should be observed for 4-6 hours after epinephrine is given to monitor for biphasic reaction. If patients are asymptomatic, they can be discharged.³
Patients who need additional doses of epinephrine are typically admitted.
Any adjunctive therapy that was started in the emergency department should be continued for 48-72 hours. Patients should be referred to an allergist and should avoid any potential triggers until allergy testing is done, this includes avoiding all peanuts and tree nuts if a nut allergy is suspected.³
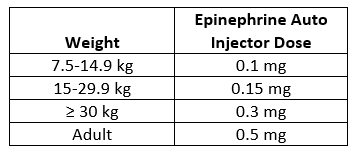
Anyone who is discharged should be prescribed an epinephrine auto injector. Instructions for use should be given prior to discharge.
Patients 7.5-14.9 kg should be prescribed 0.1 mg, 15-29.9 kg 0.15 mg, and patients 30 kg or greater should be prescribed 0.3 mg.
Auto injectors should be prescribed in two packs so that a second dose is available should symptoms return while awaiting transport to the hospital. Anyone who is given epinephrine should be evaluated in the ED.
Ideally, patients should have at least two doses available in different environments, this is especially important for children who travel between homes. However, cost may prohibit families from obtaining multiple auto injectors. If this is the case, families should ensure that the patient has epinephrine available when traveling between homes. Epinephrine auto injectors should not be left in the car.
Back to Our Patient:
As you suspected, our patient had more going on than a simple panic attack. She has more than two organ systems involved (skin, respiratory, and GI) after exposure to a food that she wasn’t sure of the ingredients. She is given 0.5 mg of 1 mg/mL (1:1,000) epinephrine IM with improvement in symptoms. After speaking with her friend who brought the cookies it is revealed that they contained macadamia nuts. Patient has never had macadamia nuts before but did have a “bad reaction” to walnuts as a child and used to have an epinephrine prescription when she was younger. She was monitored for 6 hours in the ED without return of symptoms. She was discharged home with two epinephrine auto injectors, instructions on how to use it, and instructions to avoid all tree nuts and peanuts until she is seen by an allergist.
Elizabeth Lehto, D.O.
University of Louisville | UL · Department of Pediatrics | Doctor of Pediatric Emergency Medicine
Dr. Elizabeth Lehto is a Pediatric Emergency Medicine Attending at Norton Womens and Children’s Hospital. Dr. Lehto attended Midwestern University Arizona College of Osteopathic Medicine and completed her residency and fellowship at the University of Louisville.
References
Tupper J, Visser S. Anaphylaxis: A review and update. Can Fam Physician. 2010;56(10):1009-1011.
Campbell RL, Li JT, Nicklas RA, Sadosty AT. Emergency department diagnosis and treatment of anaphylaxis: a practice parameter. Ann Allergy Asthma Immunol. 2014;113(6):599-608.
Pier J, Bingemann TA. Urticaria, Angioedema, and Anaphylaxis. Pediatr Rev. 2020;41(6):283-292.
Campbell RL, Kelso PM. Anaphylaxis: Emergency treatment. 2021; https://www.uptodate.com/contents/anaphylaxis-emergency-treatment.
Shaker MS, Wallace DV, Golden DBK, et al. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020;145(4):1082-1123.