It’s Getting Hot In Here: Heat-Related Illness
Dr. Elizabeth Lehto
Heat-related illness is caused by exposure to excessive environmental temperatures that surpass compensatory limits of thermoregulation. These illnesses are distinguished from febrile emergencies in that the increased temperature is caused by environmental heat stress, rather than a change in hypothalamic function in the setting of normothermic environmental conditions.
Presentation can range from mild (heat stress) to severe (heat stroke). Tolerance to heat varies by individual with many factors playing a role on the effect heat has on an individual including general health, overall conditioning, hydration status, and ability to acclimatize. Heat related illness is more common in the elderly and in children under 4 years old.
Pathophysiology
Body temperature is maintained within a narrow range of 97.7°F-99.5°F (36.5°C–37.5°C). The body has several processes for thermoregulation, although these processes become increasingly ineffective as ambient temperature increases.
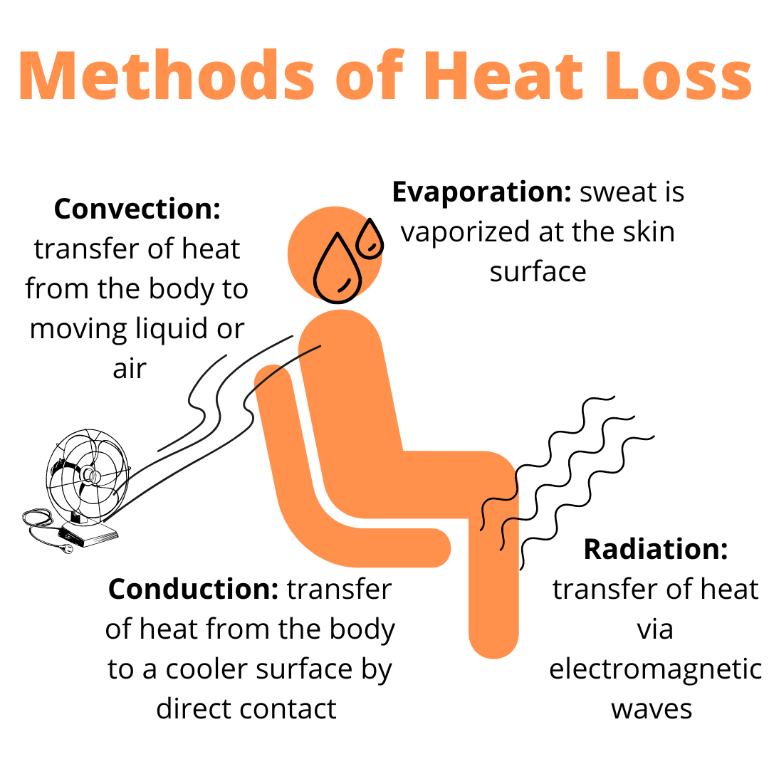
Methods of heat dissipation:
Radiation is transfer of heat from the body via electromagnetic waves (only occurs if ambient temperature is below body temperature)
Convection is transfer of heat from the body to moving liquid or ambient air
Conduction is transfer of heat from the body to a cooler surface by direct contact with the surface
Evaporation is when sweat is vaporized at the skin surface allowing heat dissipation and cooling. This is the primary methods of thermoregulation as ambient temperature increases
As the core body temperature increases, vasodilation leads to increased heart rate, stroke volume, and cardiac output. Warmer blood moves peripherally to the skin, allowing for sweat production and evaporation. As blood moves peripherally, visceral perfusion is diminished. As the body attempts to cool, high demand on the heart can progress to cardiac failure and cardiogenic shock. Hypotension often develops, commonly due to vasodilation and hypovolemia. Prolonged hypotension can lead to poor perfusion, ischemic injury, and end-organ damage.
Terminology
Heat rash/prickly heat/miliaria: erythematous popular or vesicular rash caused by obstruction of eccrine sweat glands. Commonly seen in infants during periods of high heat and humidity.
Heat edema: swelling of the feet, hands, and other dependent areas that occurs in unacclimatized individuals as a result of vasodilation and venous pooling.
Heat cramps: involuntary contractions of skeletal muscle that occurs during or after exercise. The term heat cramps is a misnomer because the heat does not directly trigger cramping and symptoms can occur during high intensity exercise in cold environments. This typically occurs in athletes that are dehydrated, deconditioned, and poorly acclimatized.
Heat syncope: brief loss of consciousness usually seen in an individual who is standing for a prolonged period or changing positions rapidly in a warm environment. Heat exposure may contribute to the event but is not the causative factor.
Heat stress: discomfort and physical strain that results from exposure to heat or warm environment. Symptoms are typically mild. Core temperature remains within the normal range.
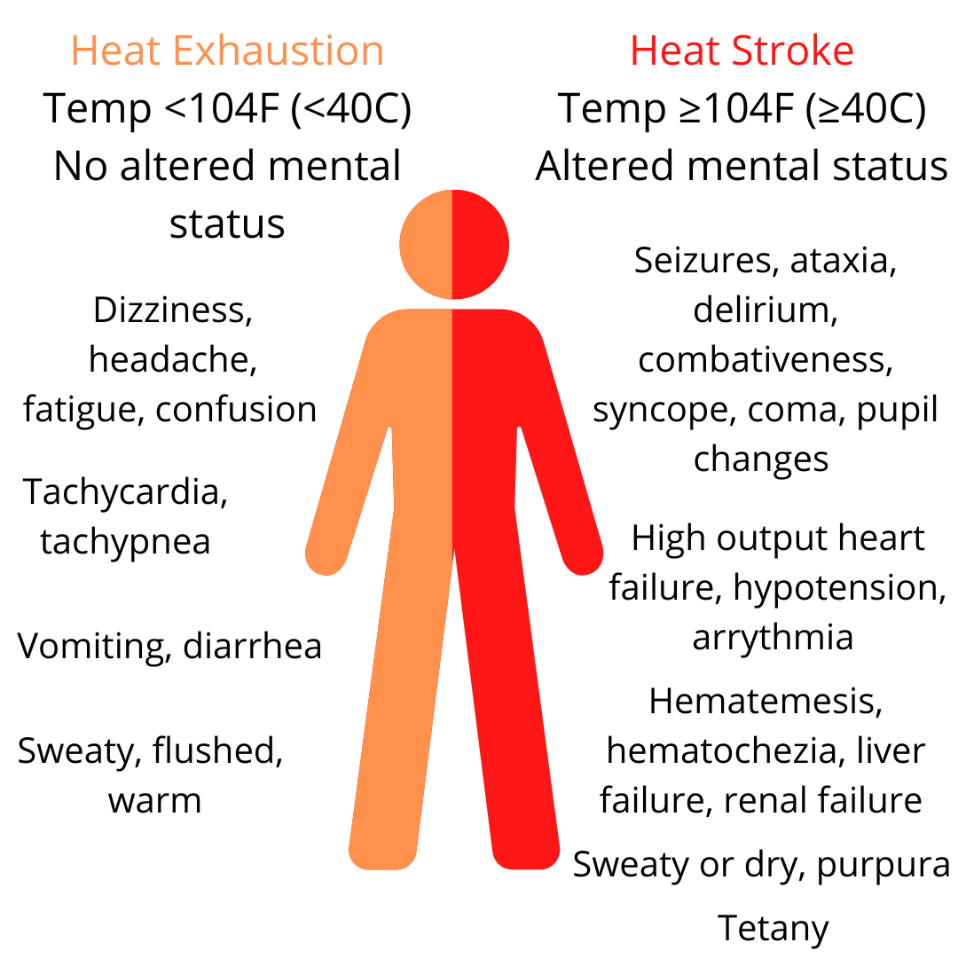
Heat exhaustion: increase in core temperature (98.6°F–104°F [37°C–40°C]). Symptoms include thirst, headache, weakness, syncope, vomiting, and dizziness. Patients are often tachycardic and hypotensive with heavy sweating. There is no central nervous system dysfunction or end-organ damage.
Heat Stroke: life-threatening condition defined as a core temperature greater than 104°F (>40°C) accompanied by central nervous dysfunction in the setting of known heat exposure and/or strenuous exercise. Central nervous system abnormalities may include agitation, confusion, delirium, or coma.
Clinical findings in heat exhaustion and heat stroke. Findings in heat exhaustion may also be present in heat stroke.
Heat stroke can be divided into two categories: exertional heat stroke and classic heat stroke. Exertional heat stroke typically occurs in those participating in strenuous sports or those whose occupations lead to heat exposure during exertion (such as firefighters). Classic heat stroke occurs among individuals who have impaired physiologic mechanisms for heat dissipation (such as metabolic or cardiac conditions) or who lack the means to escape a hot environment.
Management
Airway, breathing, and circulation should be assessed and managed appropriately. Measurement of core temperature and initiation of cooling should be the next priority once airway, breathing, and circulation have been addressed. Rectal thermometers are the gold standard for assessing core body temperature.
Cooling
Cooling must begin as soon as heat illness is suspected. First, all clothing (and equipment such as athletic gear) should be removed, and the patient should be moved to a shaded area.
Cold-water immersion is the most effective cooling method. Water temperature should be less than 60°F (<15°C) and the water should be continually stirred. The patient’s body should be fully immersed, except for the head and neck which can be covered by a wet towel.
While cold-water immersion is the most effective method, it is often not practical. Immersion makes it difficult, if not impossible, to use equipment needed to resuscitate sicker patients, including cardiac leads, intravenous equipment, and endotracheal tubes. In addition, most emergency departments do not have the facilities necessary for cold-water immersion.
The most common and effective colling method utilized in the emergency department evaporative cooling by spraying the skin with lukewarm water and using fans to maximize air circulation.
Other methods include application of cold, wet towels (that are continuously resoaked and reapplied) or placing the patient in a cold shower. Ice packs to the axilla are only marginally effective and should be used only if there are no available alternatives.
Core temperature should be continually monitored during cooing via rectal or esophageal probe. The goal of cooling is to rapidly lower the core temperature while aiming to prevent overshoot hypothermia. The threshold to stop cooling varies in the literature and ranges from 101.5°F-102°F (38.6°C–38.9°C).
Almost all patients with a heat illness will be hypovolemic. Volume replacement should occur early in the course of treatment. Normal saline is the preferred solution given high likelihood of hyponatremia after sweating profusely.
Medication
There are no specific medications indicated in the treatment of heat illness. Antipyretics are not useful in lowering core temperatures. Benzodiazepines may be considered to help control the shivering mechanism and to help prevent seizures, which may be a complication of heat stroke.
Diagnostic Testing
Testing should be based on the severity of presentation. Consider basic chemistries to assess sodium levels and renal function, creatine kinase levels for consideration of rhabdomyolysis, and coagulation parameters for assessment of disseminated intravascular coagulation. In the obtunded patient, a chest x-ray, electrocardiogram, computed tomography scan of the head, and possibly lumbar puncture should be considered to look for other causes and direct disorders arising from elevated temperature.
Prevention
Ensuring adequate oral hydration, frequent assessment at those for risk for heat illness, and avoidance of strenuous activity during temperature extremes can help prevent heat illness. Acclimatization can be highly effective in those at risk for exertional heat stroke, especially in those who cannot completely avoid heat stress for occupational reasons. Acclimatization requires daily exposure to high temperatures over a one-to-two-week period.
It is critical not to leave the elderly or young children unattended in vehicles, even for a short time with partially open windows.
Summary
Heat-related illness is due to exposure to excessive environmental temperatures that surpass the compensatory limits of thermoregulation. Early recognition and cooling is key to treatment. Cold-water immersion is the most effective means to reduce core temperature, however it is not always feasible. Evaporation techniques are more commonly used in the emergency department because they are more accessible and allow for use of other medical equipment, including cardiac monitors. Heat-related illnesses can be avoided or minimized through preventative measures such as acclimatization or, when high-temperature environments are unavoidable, reducing activities that create heat stress.
Elizabeth Lehto, D.O.
University of Louisville | UL · Department of Pediatrics | Doctor of Pediatric Emergency Medicine
Dr. Elizabeth Lehto is a Pediatric Emergency Medicine Attending at Norton Womens and Children’s Hospital. Dr. Lehto attended Midwestern University Arizona College of Osteopathic Medicine and completed her residency and fellowship at the University of Louisville.
References:
Atha W. F. (2013). Heat-related illness. Emergency medicine clinics of North America, 31(4), 1097–1108. https://doi.org/10.1016/j.emc.2013.07.012
Lugo-Amador, N. M., Rothenhaus, T., & Moyer, P. (2004). Heat-related illness. Emergency medicine clinics of North America, 22(2), 315–viii. https://doi.org/10.1016/j.emc.2004.01.004
Mangus, C. W., & Canares, T. L. (2019). Heat-Related Illness in Children in an Era of Extreme Temperatures. Pediatrics in review, 40(3), 97–107. https://doi.org/10.1542/pir.2017-0322